Company of the Month – Surgery Hero
Surgery Hero (recently re-named from Sapien Health) began life as a ‘lockdown project’ for its four co-founders and now has a vision to help 100 million people have a successful surgery. We spoke to Co-Founder and CMO, Dr Robbie Huddleston about their virtual health coaching programme for patients awaiting surgery, and how he and his fellow co-founders – Dr Matthew Beatty, Luke Eastwood and Adam Robinson – set Surgery Hero up for success.
Foundations in friendship
Surgery Hero’s founding team has history together. Before forming the company, they were all connected variously as friends, school mates, university housemates and work colleagues (even all of the above in one case). All four worked together at Huma (previously named Medopad), helping to build their remote patient monitoring platform, and had spoken about wanting to start their own business together. But how, specifically, they would best combine their backgrounds and experience in medicine, law and digital health products wasn’t clear at first. It was only during the first Covid lockdown that the inspiration finally came.
Robbie, a qualified doctor, who – prior to his stint in digital health – was specialising in A&E medicine, returned to full-time hospital work, in support of the pandemic.
“Looking back on it now, Covid ended up creating an opportunity for us. I revisited, firsthand, some of the challenges faced in patient care. Added to that, the lockdown meant we were all in our bubbles, looking for a creative outlet outside of work. It was then that all of our business ideas started coming together.”
Surgery and its challenges
Not only did the pandemic inspire the team’s creative thinking, but it also highlighted a growing need to support patients awaiting surgery. During the pandemic, waiting lists for planned procedures ballooned, and record numbers are still experiencing delays in the UK. But, as Robbie explains, even during ‘normal times’, patients waiting for surgery would benefit greatly from better support:
“There’s a misconception that going for surgery starts and ends on the day of the operation. In reality, the weeks and months before surgery can have a dramatic impact on the surgical outcome, the recovery period and long-term quality of life. In fact, while one in three people will experience some form of post-op complication, 50% of those could be avoidable with better pre-op optimization.
I often liken it to running a marathon. When you look at major surgery, the physiological trauma to the body is very similar. And I don’t know anyone who’s ever woken up and decided to run a marathon that day, without any preparation.”
A digital clinic for surgery
The Surgery Hero solution focuses on that preparation for surgery, with a view to improving the outcomes for patients.
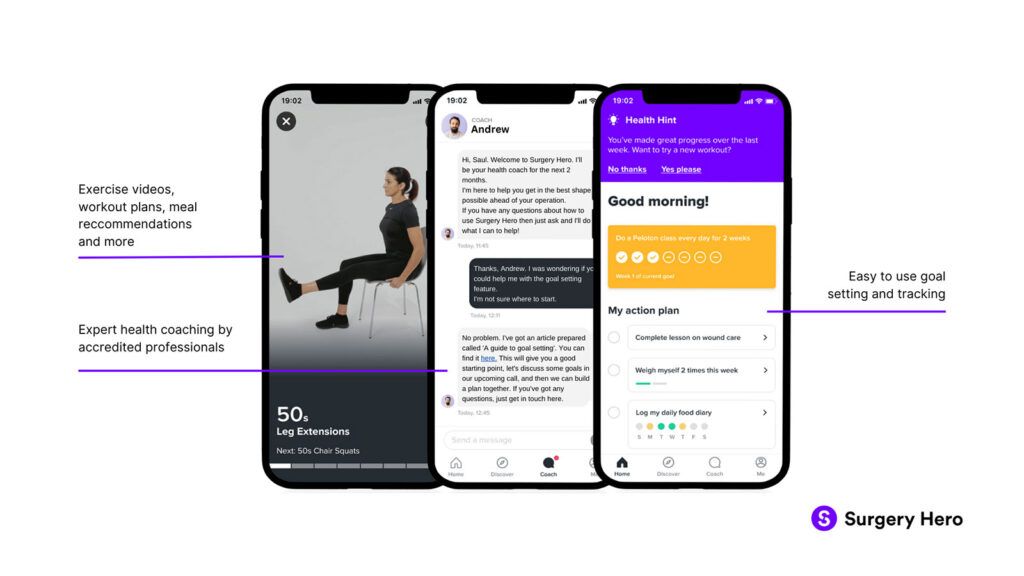
It features two key elements – self-directed learning, where the patient is provided with access to on-demand information and support, and one-to-one professional health coaching, provided remotely through their digital platform.
The self-directed learning element is tailored to an individual’s needs, objectives and risk factors. With resources such as meal plans, bite-sized learning and exercise videos, patients can access information to support common objectives, like stopping smoking or losing weight.
The one-to-one coaching is where Robbie describes their solution as unique and delivering surprising outcomes:
“I describe health coaching as the art of facilitating a person’s active participation in managing their own health. We can all relate to the concept of ‘reactance’ in psychology – where people put up barriers as soon as they feel their autonomy is being challenged. This is extremely common where patients have been advised to make behavioural changes. But health coaches are experts in behavioural change, and that’s where we really make a difference.”
As Robbie points out, the relationship formed is key to fostering behaviour change:
“We don’t refer to our users as ‘patients’, because this can infer a dictatorial relationship. We have ‘members’ because what we’re doing is very much a collaboration between coach and member.”
Once enrolled, every Surgery Hero member gets paired with their own health coach. They stay in contact throughout the programme via in-app messaging, phone call, video call or a combination of each.
The ideal scenario Robbie describes is an eight-week pre-op programme, followed by four weeks of post-op support, though this can vary depending on fluctuating waiting lists, type of procedure and local needs. Even with just two to four weeks of pre-op support, he says they have seen impressive outcomes.
Outcomes
With outcomes in mind, the team are now excited to be working on their first randomised control trial across Sherwood Forest and Royal Berkshire hospitals, for hip and knee replacement surgery. The trial is an extension of research at South Tees Hospitals, where they were able to demonstrate patients’ average post-op hospital stay being reduced by a full day (equating to a cost saving of £275 for every patient).
Those outcomes also look likely to translate into longer-term benefits and cost savings, when looking at the Patient Activation Measure (PAM) for members before and after the programme. PAM measures people’s knowledge, skills and confidence in managing their own wellbeing, on a 100-point scale. Surgery Hero has been able to demonstrate a consistent cohort-wide improvement in PAM scores of around 10 points. And, the improvements they see are even greater for those that start at a lower base.
PAM scores can be simplified down to four ‘activation’ levels, where levels one and two broadly describe ‘non-activated’ patients, and levels three and four ‘activated’. What the trial showed was that 71% of members in the non-activated groups were in an activated group, following their coaching programme:
“People who fall into levels one and two have higher rates of unplanned health care utilisation, engage in fewer preventative behaviours, and they’re generally much more costly to the NHS. If you’re looking at the systems level, shifting people out of those ‘non-activated’ groups is where the wider NHS benefits most. Typically, that shift in behaviour is long term – up to 18 months without further intervention – so what we’ve demonstrated is something that potentially means long-term benefit, both to the individual and the NHS as a whole.”
Growth
With these promising outcomes demonstrated, the Surgery Hero team has been growing rapidly since they became fully operational in early 2021. They now have four full-time health coaches, which they expect to double by Q2 this year, and they are also growing their product design, engineering and sales capacity.
This growth follows successful pre-seed and seed funding rounds late last year, where they raised £2.5 million, led by LifeArc Ventures and SFC Capital, including Crista Galli Ventures and Clarendon Fund Managers.
A number of accelerators have also supported their growth story. From the Oxford AHSN Accelerator and East Midlands AHSN Digital Health Accelerator, to (most recently) the DigitalHealth.London Accelerator and AWS Expand programme. Robbie also cites the NHS Clinical Entrepreneur Programme as being valuable to him personally.
They’ve also tapped into further support by making use of the Evidence Canvas MedCity has designed to help SMEs map out the evidence they need to advance commercialisation, as well as gaining support in networking and introductions:
“The Evidence Canvas has been really helpful for adding structure to our evidence generation process – giving clarity to our strategy and what we’re looking to achieve. And the introductions have also been invaluable. In fact, it was via MedCity that we were introduced to Imran Hamid, Senior Investment Principle at LifeArc – and they went on to be our largest single investment.”
Overcoming challenges
Despite the support schemes and funding success, Robbie is happy to accept that selling into the NHS has its challenges. With large, complicated organisations, and a high bar for risk management and information governance, many startups struggle. One of the ways the founding team has overcome these challenges is to focus on governance and compliance upfront. As well as Robbie heading up clinical safety, co-founder Luke Eastwood oversees information governance, and they’ve taken a thorough approach to developing their procedures for all compliance issues:
“It took a lot of effort up front, but we essentially have a dossier that we can provide to NHS organisations, covering all the compliance issues that can come up in contract and pre-contract conversations. That’s really helped smooth over and speed up those discussions.”
That effort seems to have paid off for the team. They are currently working with seven NHS Trusts, including those research projects mentioned above, plus a study at Portsmouth Hospitals University NHS Trust, and live services in three separate integrated care systems.
With this success under their belts, the foreseeable future will be spent focusing on expanding into more NHS organisations, and within those they’re already working with. With applications across all types of surgery and procedures, the possibilities seem almost limitless.
Find out more: surgeryhero.com
For access to the Evidence Canvas and our upcoming workshop, please get in touch here.